Cranioplasty: Optimizing Clinical and Cosmetic Outcomes for Cranial Defects
Craig H. Lichtblau1, Scott Raffa2, Kaveh Assadi3, Christopher Warburton4, Gabrielle Meli5, and Allyson Gorman6
1Medical Director, Osseointegration Program, Physical Medicine and Rehabilitation Consultant to the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, FL, USA, Consultant to Children’s Medical Services for the State of Florida, District 9, St. Mary’s Medical Center; 2Neurosurgeon, Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, FL, USA; 3Pediatric Neurosurgeon, Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, FL, USA; 4University of Miami Miller School of Medicine, Miami, FL, USA; 5University of Miami Miller School of Medicine, Miami, FL, USA; 6Medical College of Wisconsin, Wauwatosa, Wisconsin, USA
ABSTRACT
In addition to its aesthetic benefits, cranioplasty has been shown to improve neurological symptoms related to cranial defects. Here we describe a case study from a cranioplasty procedure performed 3 decades ago and discuss subsequent research that has helped to clarify the benefits we have observed in those who have undergone cranioplasty.
Keywords: Cranioplasty; Craniotomy; Neurological symptoms; Cranial defects
INTRODUCTION
Cranioplasty is a reconstructive neurosurgery that repairs cranial defects. The concept behind cranioplasty has been practiced as far back 3000 B.C., when the Incas covered trauma-induced cranial defects with gold [1-3]. The procedure was once performed largely to restore normal appearance, but it was eventually recognized that cranioplasty also provides clinical benefits and should thus be used not only as a cosmetic procedure but also as a therapeutic one [2,4,5].
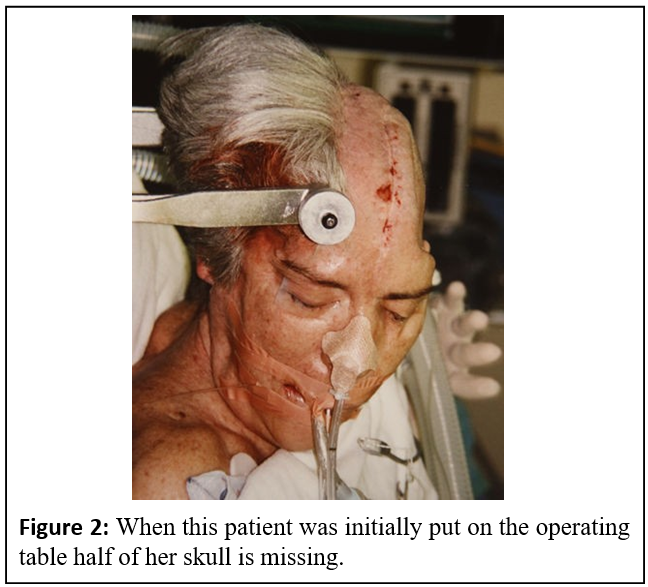
In addition to improving aesthetic and clinical outcomes, cranioplasty can also enhance the success and efficiency of the rehabilitation process. Here we briefly describe our observations following cranioplasty performed 30 years ago and compare those results with data that have since emerged and that have helped to corroborate our anecdotal data on both the direct benefits of cranioplasty and the indirect benefits that occur through cranioplasty-facilitated rehabilitation. 30 years ago, we observed cranioplasty catapult the rehabilitation process. By the 1940s, clinicians began describing improvements in neurological symptoms following cranioplasty, but for decades, little research was conducted on the link between this correction of skin flap depression following cerebral decompression and changes in symptoms [6]. In 1992, we treated a 63-year old white female who had been hit by a motor vehicle while walking and sustained a comminuted fracture on the right side of her skull as well as multiple other skull fractures.
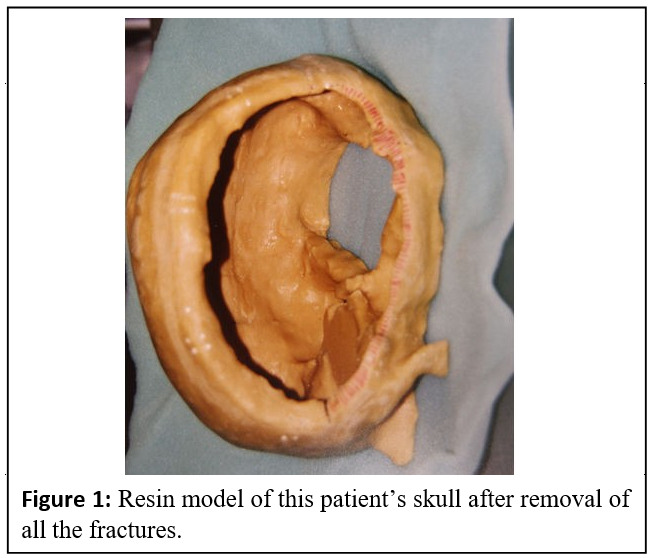
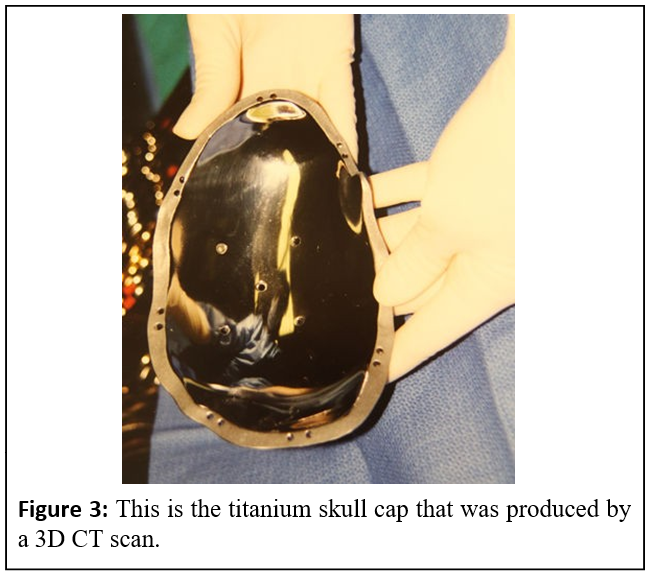
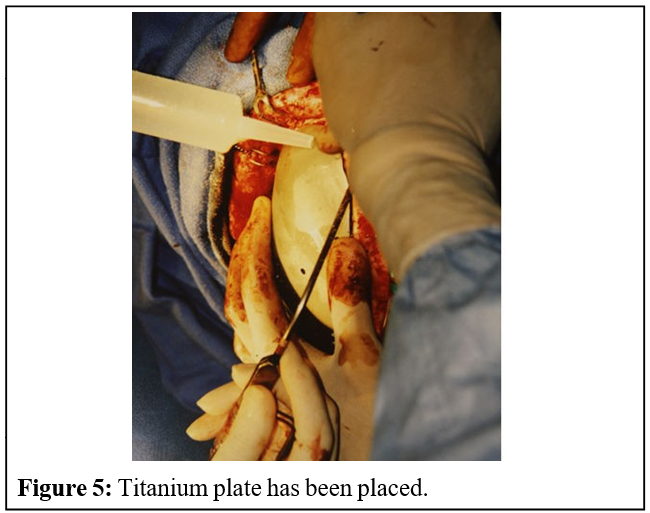
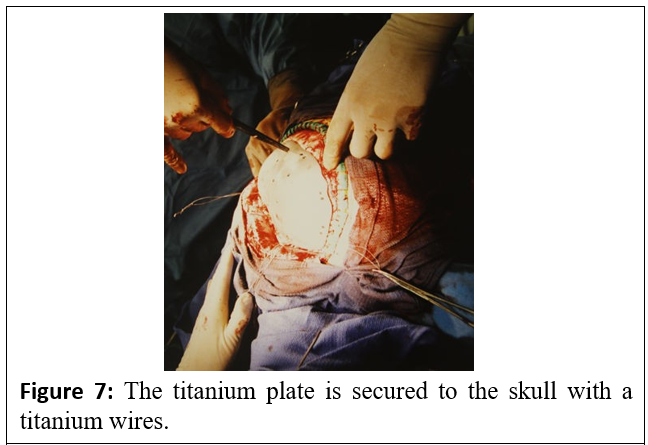
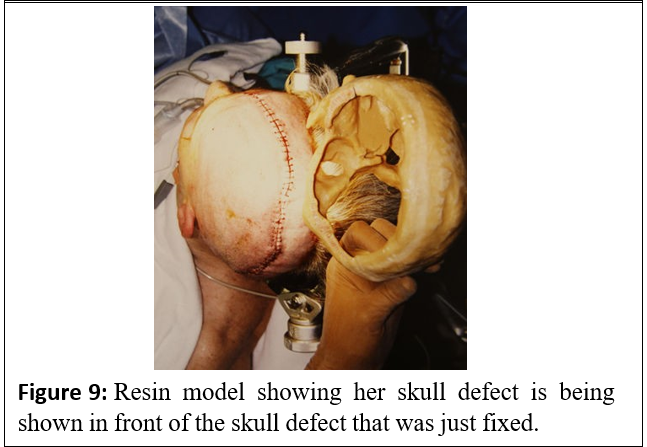
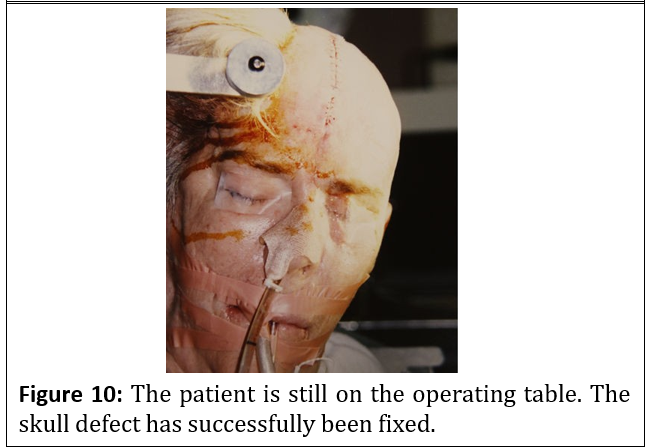
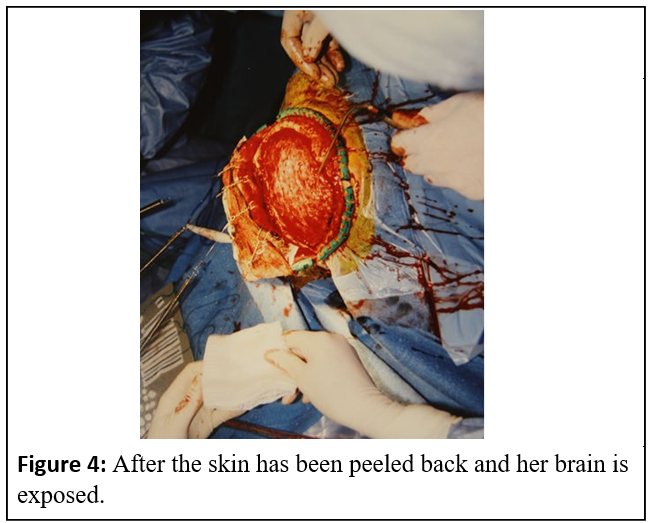
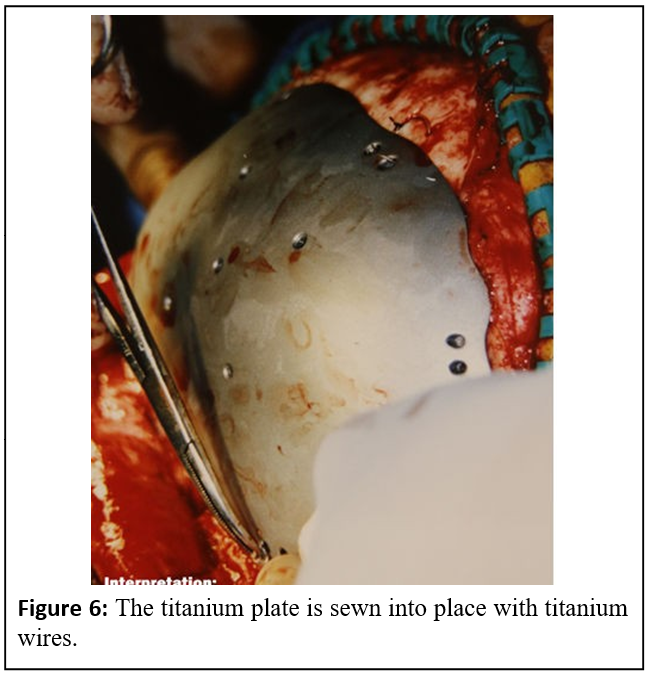
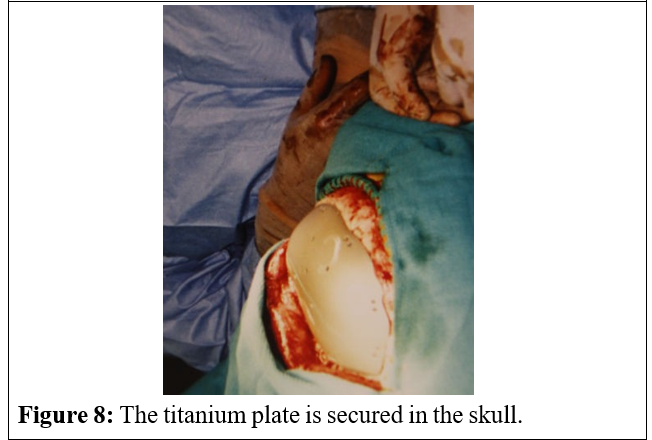
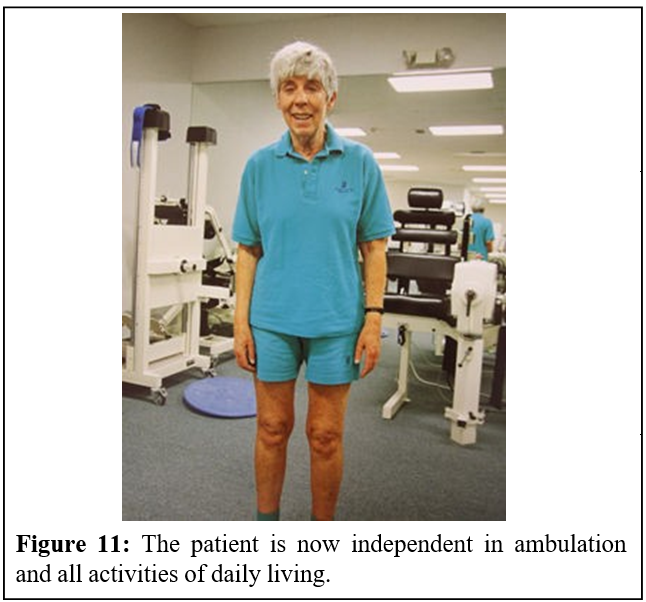
The patient was neurologically devasted following the removal of shattered cranial bones, and she required 24-hour daily aide and attendant care. She was unable to participate in an inpatient rehabilitation program, as she had no physical or cognitive capacity. The patient’s body rejected the implantation of stainless-steel mesh and methyl methacrylate that was inserted to fix her skull defect. A second attempt at cranioplasty was undertaken by formulating a titanium skull cap using a 3- dimensional computed tomography scan. After two neurosurgeons worked together to surgically place the cap, the patient demonstrated marked improvement in both her physical and cognitive abilities. These improvements that were observed following cranioplasty enabled the patient to participate in an aggressive inpatient rehabilitation program for 4 weeks. She was then able to ambulate independently, resume her activities of daily living, and reintegrate back into society. Cranioplasty- related images can be viewed in the supplementary material (Figures 1-11).
Correspondence to: Craig H. Lichtblau, Physical Medicine and Rehabilitation Consultant to the Paley Orthopedic and Spine Institute, St. Mary’s Medical Center, West Palm Beach, Florida, USA, E-mail: c.lichtblau@chlmd.com
Received: 03-Dec-2022, Manuscript No. JPMR-23-20802; Editor assigned: 06-Dec-2022, PreQC No. JPMR-23-20802 (PQ); Reviewed: 21-Dec-2022, QC No. JPMR-23-20802; Revised: 28-Dec-2022, Manuscript No. JPMR-23-20802 (R); Published: 05-Jan-2023, DOI: 10.35248/2329-9096.23.11.655
Citation: Lichtblau CH, Warburton C, Meli G, Gorman A (2023) Cranioplasty: Optimizing Clinical and Cosmetic Outcomes for Cranial Defects. Int J Phys Med Rehabil. 11:655.
Copyright: © 2023 Lichtblau CH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Though the role of cranioplasty in her recovery was clear, there was little evidence from systematically conducted research on the specific benefits of cranioplasty and the mechanisms by which cranioplasty reversed neurological symptoms. Fortunately, much has since come to light on the contexts in which cranioplasty is appropriate and the specific ways it can best be used to help patients recover from trauma.
LITERATURE REVIEW
Cranioplasty is performed worldwide following decompressive craniectomy
Complications of decompressive craniectomy, which is regularly pursued as a surgical solution for increased intracranial pressure that does not respond to other treatments, have helped to demonstrate the benefits of cranioplasty [7]. Randomized, prospective clinical trials have shown how decompressive craniectomy can prevent complications associated with brain edema that result from trauma, stroke, infection, or other causes and is performed using a patient’s autologous skull flap [7,8]. While valuable, decompressive craniectomy is associated with risks of trephined syndrome and sinking flap syndrome [5]. Trephined syndrome refers to sunken skin above the bone defect that is accompanied by neurological symptoms including headaches, dizziness, seizures, cognitive and psychiatric changes, or sensorimotor deficits [1,6,9]. Similarly, sinking flap syndrome involves neurological symptoms that arise because of concavity of the skin flap and the resulting pressure on underlying brain tissue [10].
Because cranioplasty helps to address and treat both trephined syndrome and sinking flap syndrome, it is regularly employed following decompressive craniectomy [7,11]. Though decompressive craniectomy may be used for several reasons, it is often employed in response to accidental trauma or violence. With improvements in trauma care, the volume of decompressive craniectomy procedures have grown and thus so too has the volume of cranioplasties [6,7].
Cranioplasty provides clinical value through multiple mechanisms
It is now well-established that cranioplasty offers an effective solution for restoring normal contour for aesthetic purposes while also providing critical cerebral protection and potentially reversing a host of neurological symptoms [2]. In addition to motor recovery and neuropsychological recovery, cognitive recovery has been observed immediately following cranioplasty [12]. Cranioplasty has also been shown to improve cardiovascular functions [13]. The improvements in functioning and appearance that accompany cranioplasty have been cited as contributing to boosts in patients’ self-esteem and overall quality of life [7,9].
The reversal of neurological symptoms that accompany cranioplasty are thought to occur because of a reduction in atmospheric pressure and thus a concomitant reduction in local cerebral compression.4 These pressure changes appear to significantly affect the hydrodynamics of Cerebrospinal Fluid (CSF), which may increase CSF cranial coverage and thereby help to restore neurological function, through for instance, restored communication among neuronal networks [14,15]. Restoration of cerebral hemodynamics resulting from these pressure changes may also enhance cerebral blood flow and metabolism, improving cerebral blood perfusion and reversing a range of symptoms [1,16-18]. Though many people benefit significantly from cranioplasty, there is some variability in the amount of functional improvement across patient populations. Research into the specific benefits of cranioplasty has revealed that while age, sex, type of injury, and side of craniectomy are not associated with rate of functional improvement, those suffering disorders of consciousness show more significant gains than those without such disorders [19]. Further, those with brain midline shift show more significant consciousness improvements following cranioplasty than those without a brain midline shift [4]. Fortunately, the clinical benefits of cranioplasty appear to persist, as Traumatic Brain Injury (TBI) patients evaluated a full year after cranioplasty continue to demonstrate favorable outcomes [20]. Early intervention is likely advantageous, as least in certain contexts. Determining the best time to perform cranioplasty requires balancing the need for cranioplasty’s clinical benefits with the need for the patient’s brain to first recover from the trauma. Though the optimal timing for cranioplasty is controversial, much of the literature suggests that between 3 and 6 months following decompressive craniectomy is an ideal time to pursue cranioplasty to achieve cognitive and motor recovery [21]. Some researchers have suggested that early intervention with cranioplasty may enhance its benefits [22,23]. For instance, patients whose cranioplasties were performed within 6 months of injury have been shown in certain cases to reap greater cognitive benefits than those whose cranioplasties were delayed past 6 months [23]. There is also evidence that patients who have undergone decompressive craniectomy for management of intracranial hypertension may benefit from early cranioplasty [8,24].
Despite recommendations for early intervention, there is also some evidence for a lack of connection between procedure timing and recovery that suggests that cranioplasty does not need to be planned to take advantage of a specific window of opportunity related to rehabilitation [10]. Research suggesting that cranioplasty timing is not critical for optimizing outcomes includes data showing that those receiving cranioplasty an entire year after their injury demonstrate the same benefits as those undergoing the procedure only a few months following their injury [12,22]. Other data have shown that those who wait up to 3 years following TBI to undergo cranioplasty experience comparable cognitive improvements to those whose cranioplasties were more urgently performed [15].
Though the potential advantages of early intervention with cranioplasty continues to be debated, researchers suggest that prompt intervention with this procedure should be considered in the face of large craniectomy defects, particularly given the rapid and dramatic cognitive and neurological recovery that is often observed following the procedure [5,7,10]. It is also possible that delaying cranioplasty may enhance the risk for certain complications, such as post-surgical seizures, which provides further support to the notion that early intervention may lead to better outcomes than later intervention [25].
Optimizing cranioplasty procedures may reduce surgery-related complications
Because cranioplasty is technically complex and requires highly trained technicians, failures occur [26]. Developing a customized plan that is tailored to the specific needs of the patient is critical for improving the success rate of these procedures. This process can also help in managing patients’ risk factors and in enabling early identification and intervention when complications arise [27]. Infection at the surgical site is a common complication associated with cranioplasty, occurring in up to 1 in 5 patients [1]. Another well-known complication that is particularly common in pediatric patients is the resorption of the bone flap. Both complications are more likely in TBI patients than in those undergoing the procedure for other indications [28].
DISCUSSION
Though most complications involve infections, convulsions and epidural hematoma, brain hemorrhage and edema can occur and may lead to death [29]. Hydrocephalus may occur due to a decompressive craniectomy procedure or from intraventricular or subarachnoid hemorrhage [1]. There have been advancements in recent years to improve the materials used for cranioplasty to reduce the risk of infection by for instance, increasing antimicrobial activity of the material with elevated intracellular free levels of calcium [30]. While cranioplasties can employ biological materials or synthetic materials, certain materials have fallen out of favor because they are associated with complications like infection, rejection, and resorption [1,2]. Autologous cranioplasty is therefore the most common cranioplasty technique and employs bone from the patient’s own body. Much of the technical detail of cranioplasty depends on the surgeon’s preferences [31]. However; the gold standard for cranial defect reconstruction has become Custom Made Cranioplasty (CM CPL) that targets an effective combination of brain protection and cosmetic benefits. It is important to note, though, that CM CPL is expensive, and prosthesis preparation is time consuming [32]. The ideal material for cranioplasty procedures is one that will fit the cranial defect properly, allowing for complete closure, while also resisting infection, being conducive to contouring, and being as strong as the surrounding bone [33]. Scientific advancements have made it easier than ever before to develop the best prosthesis for each patient and to perform cranioplasty in a way that will provide maximum clinical benefit in the context of that patient’s injury and health status [34-36].
CONCLUSION
Since our observation of dramatic clinical benefits following cranioplasty 30 years ago, the procedure has become a commonly utilized neurosurgical technique for skull reconstruction, with significant benefits in relevant technology aiding its use over the past couple of decades. As in our experience, the evidence suggests that it is critical to personalize care to ensure the best approach-including optimal materials and timing-is undertaken to increase the chances of success and optimize health outcomes.
REFERENCES
- Alkhaibary A, Alharbi A, Alnefaie N, Almubarak AO, Aloraidi A, Khairy S. Cranioplasty: A comprehensive review of the history, materials, surgical aspects, and complications. World neurosurg. 2020; 139:445-52.
- Mostafa Elkatatny AAA, Eldabaa KA. Cranioplasty: A New Perspective. Open Access Maced J Med Sci. 2019; 7(13):2093.
- Andrabi S, Sarmast A, Kirmani A, Bhat A. Cranioplasty: Indications, procedures, and outcome: An institutional experience. Surg Neurol Int. 2017; 8(1):91.
- Lin CH, Yang JT, Wang TC, Lin MHC, Cheng WC, Lee MH. Is preoperative brain midline shift a determinant factor for neurological improvement after cranioplasty? J Formos Med Assoc. 2015; 114(7): 577-582.
- Jeyaraj P. Importance of Early Cranioplasty in Reversing the Syndrome of the Trephine/Motor Trephine Syndrome/Sinking Skin Flap Syndrome. J Maxillofac Oral Surg. 2015; 14(3):666.
- Alibhai MK, Balasundaram I, Bridle C, Holmes SB. Is there a therapeutic role for cranioplasty? Int J Oral Maxillofac Surg. 2013; 42(5):559-561.
- Cho YJ, Kang SH. Review of Cranioplasty after Decompressive Craniectomy. Korean J Neurotrauma. 2017; 13(1):9.
- Archavlis E, Carvi Y Nievas M. The impact of timing of cranioplasty in patients with large cranial defects after decompressive hemicraniectomy. Acta Neurochir (Wien). 2012; 154(6):1055-1062.
- Corallo F, Calabró RS, Leo A, Bramanti P. Can cranioplasty be effective in improving cognitive and motor function in patients with chronic disorders of consciousness? A case report. Turk Neurosurg. 2015; 25(1):193-196.
- Di Stefano C, Sturiale C, Trentini P, Bonora R, Rossi D, Cervigni G, et al. Unexpected neuropsychological improvement after cranioplasty: a case series study. Br J Neurosurg. 2012; 26(6):827-831.
- Schiffer J, Gur R, Nisim U, Pollak L. Symptomatic patients after craniectomy. Surg Neurol. 1997; 47(3):231-237.
- Corallo F, de Cola MC, Lo Buono V, Marra A, de Luca R, Trinchera A, et al. Early vs late cranioplasty: what is better? Int J Neurosci. 2017; 127(8):688-693.
- Won YD, Yoo DS, Kim KT, Kang SG, Lee SB, Kim DS, et al. Cranioplasty effect on the cerebral hemodynamics and cardiac function. Acta Neurochir Suppl. 2008; 102(102):15-20.
- Honeybul S, Janzen C, Kruger K, Ho KM. The impact of cranioplasty on neurological function. Br J Neurosurg. 2013; 27(5): 636-641.
- Jelcic N, Puppa DA, Mottaran R, Cecchin D, Manara R, Dam M, et al. Case series evidence for improvement of executive functions after late cranioplasty. Brain Inj. 2013; 27(13-14):1723-1726.
- Corallo F, lo Buono V, Calabrò RS, de Cola MC. Can Cranioplasty Be Considered a Tool to Improve Cognitive Recovery Following Traumatic Brain Injury? A 5-Years Retrospective Study. J Clin Med. 2021;10(22).
- Shahid AH, Mohanty M, Singla N, Mittal BR, Gupta SK. The effect of cranioplasty following decompressive craniectomy on cerebral blood perfusion, neurological, and cognitive outcome. J Neurosurg. 2018; 128(1):229-235.
- Halani SH, Chu JK, Malcolm JG, Rindler RS, Allen JW, Grossberg JA, et al. Effects of Cranioplasty on Cerebral Blood Flow Following Decompressive Craniectomy: A Systematic Review of the Literature. Neurosurgery. 2017; 81(2):204-216.
- Jasey N, Ward I, Lequerica A, Chiaravalloti ND. The therapeutic value of cranioplasty in individuals with brain injury. Brain Inj. 2018; 32(3):318-324.
- Posti JP, Yli-Olli M, Heiskanen L, Aitasalo KM, Rinne J, Vuorinen V, et al. Cranioplasty after severe traumatic brain injury: Effects of trauma and patient recovery on cranioplasty outcome. Front Neurol. 2018; 9:223.
- de Cola MC, Corallo F, Pria D, lo Buono V, Calabrò RS. Timing for cranioplasty to improve neurological outcome: A systematic review. Brain Behav. 2018; 8(11):e01106.
- Malcolm JG, Rindler RS, Chu JK, Chokshi F, Grossberg JA, Pradilla G, et al. Early Cranioplasty is Associated with Greater Neurological Improvement: A Systematic Review and Meta-Analysis. Neurosurgery. 2018; 82(3):278-288.
- Stefano CD, Rinaldesi ML, Quinquinio C, Ridolfi C, Vallasciani M, Sturiale C, et al. Neuropsychological changes and cranioplasty: A group analysis. Brain Inj. 2016; 30(2):164-171.
- Bender A, Heulin S, Röhrer S, Mehrkens JH, Heidecke V, Straube A, et al. Early cranioplasty may improve outcome in neurological patients with decompressive craniectomy. Brain Inj. 2013; 27(9): 1073-1079.
- Shih FY, Lin CC, Wang HC, Ho JT, Lin CH, Lu YT, et al. Risk factors for seizures after cranioplasty. Seizure. 2019; 66:15-21.
- Sahoo NK, Tomar K, Thakral A, Kumar S. Failures in cranioplasty: A clinical audit & review. J Oral Biol Craniofac Res. 2021; 11(1):66.
- Zanaty M, Chalouhi N, Starke RM, Clark SW, Bovenzi CD, Saigh M, et al. Complications following cranioplasty: incidence and predictors in 348 cases. J Neurosurg. 2015; 123(1):182-188.
- Shepetovsky D, Mezzini G, Magrassi L. Complications of cranioplasty in relationship to traumatic brain injury: A systematic review and meta-analysis. Neurosurg Rev. 2021; 44(6):3125-3142.
- Kato A, Morishima H, Nagashima G. Unexpected complications immediately after cranioplasty. Acute Med Surg. 2017; 4(3):316-321.
- Mommaerts MY, Depauw PR, Nout E. Ceramic 3D-Printed Titanium Cranioplasty. Craniomaxillofac Trauma Reconstr. 2020;13(4):329-333.
- Zanotti B, Zingaretti N, Verlicchi A, Robiony M, Alfieri A, Parodi PC. Cranioplasty: Review of Materials. J Craniofac Surg. 2016; 27(8):2061-2072.
- Zoli M, di Gino M, Cuoci A, Palandri G, Acciarri N, Mazzatenta
D. Handmade Cranioplasty: An Obsolete Procedure or a Surgery That Is Still Useful? J Craniofac Surg. 2020; 31(4):966-972. - Khader BA, Towler MR. Materials and techniques used in cranioplasty fixation: A review. Mater Sci Eng C Mater Biol Appl. 2016; 66:315-322.
- Mee H, Anwar F, Timofeev I, Owens N, Grieve K, Whiting G, et al. Cranioplasty: A Multidisciplinary Approach. Front Surg. 2022; 9.
- Piazza M, Grady MS. Cranioplasty. Neurosurg Clin N Am. 2017; 28(2):257-265.
- Su JH, Wu YH, Guo NW, Huang CF, Li CF, Chen CH, et al. The effect of cranioplasty in cognitive and functional improvement: Experience of post traumatic brain injury inpatient rehabilitation. Kaohsiung J Med Sci. 2017; 33(7):344-350.
