Evidence Based Methodology to Predict Successful Surgical Outcomes Utilizing Lumbar Microdiscectomy in Patients that Have Failed Conservative Treatment

Craig H Lichtblau1*, Corey B Fuller2, David R. Campbell3
1Physical Medicine and Rehabilitation Consultant to the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, Florida, USA;2Department of Orthopedic Surgery, Loma Linda University, Loma Linda, California, USA;3Department of Orthopedic Surgery, University of Central Florida College of Medicine, Orlando, Florida, USA.
ABSTRACTObjectives: The most common culprit of lower back pain with radiculopathy is degeneration of the intervertebral space leading to disc disease and lumbar disc herniation (LDH). Management of LDH with radiculopathy consists of anti-inflammatories medications, local corticosteroid injections, physical therapy and surgery. Preoperative symptoms, physical exam findings and MRI findings, including herniation size, are all commonly used to determine appropriate surgical candidates.
Methods: This study is a retrospective analysis of 8 patients who underwent microdiscectomy for LDH with radicular symptoms looking at symptoms, physical exam findings and disk herniation volume on MRI and intraoperatively. All patients underwent questionnaire of preoperative characteristics of pain, radicular specific physical exam findings and LDH volume via preoperative lumbar spine MRI imaging as well as intra-operative disk volume removed at time surgery. Data was analyzed retrospectively see if LDH volume correlated with preoperative symptoms or exam findings and postoperative outcome.
Results: All patients with significant frequency, duration, intensity and radicular pattern of pain had significant improvement in radicular pain postoperatively. Preoperative MRI disc volume did not correlate with actual intraoperative disk volume removed 63% of the time. MRI findings of disk size poorly correlated with physical exam findings. Actual surgical volume of disk size correlated with preoperative physical exam findings. No patients with small surgical volume of intra-operative disk had any loss of motor, sensation or deep tendon reflexes measured preoperatively. 40% of large intra-operative disk volume removed had affected physical exam findings preoperatively.
Conclusion: Preoperative MRI, physical exam findings and disc size at the time of surgery does not correlate well with the probability of a good surgical outcome provided that there was no clinically significant psychological factors and functional issues. Frequency, duration, intensity and radicular pattern of pain in failed conservative treatment are more reliable predictors of surgical success of surgical success.
Keywords: Lower back pain; Anti-inflammatories medications; Lumbar spine; MRI
INTRODUCTION
It is estimated that 80% of the population will experience lower back pain once in their lifetime [1]. Lower back pain with or without radiculopathy is frequently initially treated by family medicine, internal medicine or physical medicine and rehabilitation physicians and is the fifth most common reason for doctor visits nationwide [2]. The most common culprit of lower back pain with radiculopathy is degeneration of the intervertebral space leading to disc disease and lumbar disc herniation (LDH) [3].
Correspondence to: Craig H Lichtblau, Physical Medicine and Rehabilitation Consultant to the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center. West Palm Beach, Florida, USA, Tel: 561-842-3694; E-mail: c.lichtblau@chlmd.com
Received date: April10, 2020; Accepted date: April 20, 2020; Published date: April 27, 2020
Citation: Lichtblau CH, Fuller CB, Campbell DR (2020) Evidence Based Methodology to Predict Successful Surgical Outcomes Utilizing Lumbar Microdiscectomy in Patients that Have Failed Conservative Treatment.
Copyright: © 2020 Lichtblau CH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Management of lumbar disc herniation with radiculopathy is largely conservative consisting of anti-inflammatories medications, local corticosteroid injections and physical therapy, however surgical management does play an important role. This study is a retrospective analysis of 8 patients who underwent lumbar microdiscectomy for lumbar disc herniation with radicular symptoms.
MATERIALS AND METHODS
From 2012-2020 the senior author (C.L) referred 80 patients with lumbar disc herniation and radicular symptoms for surgical decompression. These 80 patients underwent laminectomy with microdiscectomy by a Board-Certified Fellowship Trained Spine Surgeon, Dr. David Campbell. Of these 80, eight of these patients had the excised portion of the intervertebral disc herniation photographed intra-operatively and are the focus of this study.
These eight patients all had lumbar spine magnetic resonance imaging (MRI) that confirmed lumbar disk herniation. Three
Kim [4]. Based on this, four patients had LDHs classified as small and four had LDHs that were classified as large.
All eight patients had undergone a detailed preoperative history that included questions about pain frequency, duration, intensity and pattern. All patients described pain as a constant radicular pain in one or both legs in a dermatomal pattern that was concordant with the level of their disk pathology. All eight patients endorsed their radicular pain intensity as significant (>7/10) with a duration of greater than 6 months. Radicular pain was significantly affecting quality of life in all patients without improvement despite conservative management. As part of their preoperative evaluation, all eight patients had undergone a detailed physical exam with sensory, motor and deep tendon reflexes recorded. See Table 1 for preoperative physical examination findings.
All patients eventually underwent lumbar microdiscectomy by a board-certified fellowship trained orthopedic spine surgeon. At the time of surgery, the entire part of
Laminectomy MRI Disk MRI Physical Physical +Microdiscectomy Pathology Disk Exam Exam (Small) Pathol (Motor (Motor ogy Strength) Strength) (Large) (Decreased) (Normal)
| Laminectomy MRI Disk MRI Physical Physical +Microdiscectomy Pathology Disk Exam Exam (Small) Pathol (Motor (Motor ogy Strength) Strength) (Large) (Decreased) (Normal) |
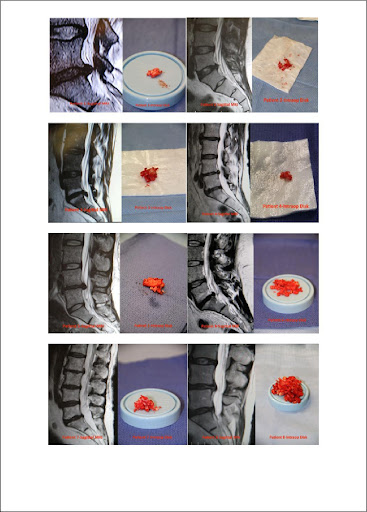
patients had herniations at the L4-L5 disc, four had herniations at the L5-S1 disc and one patient had herniations at both the L4-L5 and L5-S1 disc spaces. Disk herniations were classified as small if the herniation measured <6 mm on MRI imaging and as large if the herniation was >6 mm as described by Carragee and the disc that was herniated was excised and the volume of intervertebral disk removed and photographed. See Figure 1 for sagittal MRI images and photographs of intraoperative disk removed. The principal author (C.L) assisted in 80 lumbar microdiscectomies and in eight of the cases selected at random, the disc volume the disk volume removed was photographed and recorded.
Table 1: Eight Case Correlation.
Kim [4]. Based on this, four patients had LDHs classified as small and four had LDHs that were classified as large.
All eight patients had undergone a detailed preoperative history that included questions about pain frequency, duration, intensity and pattern. All patients described pain as a constant radicular pain in one or both legs in a dermatomal pattern that was concordant with the level of their disk pathology. All eight patients endorsed their radicular pain intensity as significant (>7/10) with a duration of greater than 6 months. Radicular pain was significantly affecting quality of life in all patients without improvement despite conservative management. As part of their preoperative evaluation, all eight patients had undergone a detailed physical exam with sensory, motor and deep tendon reflexes recorded. See Table 1 for preoperative physical examination findings.
All patients eventually underwent lumbar microdiscectomy by a board-certified fellowship trained orthopedic spine surgeon. At the time of surgery, the entire part of the disc that was herniated was excised and the volume of intervertebral disk removed and photographed. See Figure 1 for sagittal MRI images and photographs of intraoperative disk removed. The principal author (C.L) assisted in 80 lumbar microdiscectomies and in eight of the cases selected at random, the disc volume the disk volume removed was photographed and recorded.
PROCEDURE
L4-L5+++++
L5-S1+++++
L5-S1+++++
L4-L5+++++
L4-L5+++++
L5-S 1+++++
L5-S 1+++++
L4-L5+L5-S1+++++
Pathology
(Volume)PhysicalPhysicalPhysicalPhysical ExamSmallLargeExamExamExam(Deep TendonVolum Volum(Sensory)(Sensory)(DeepReflex)ee(Decrease d)(Normal)Tendon Reflex)(Normal)
(Decreased)
RESULTS
At follow-up all eight patients had significant improvement in radicular pain postoperatively compared to preoperative symptoms.
Intervertebral disc volume based on pre-operative MRI did not correlate with actual intra- operative intervertebral disc volume removed 63% of the time (5/8 cases). This represented 3/8 (38%) where preoperative MRI underestimated the actual disk volume
requiring excision intraoperatively and 2/8 (25%) where MRI overestimated disk volume requiring excision intraoperatively.
MRI findings of intervertebral disk size poorly correlated with physical exam findings.
In the 4 patients with large disk involvement measured on preoperative MRI, all patients had normal motor, sensation and deep tendon reflexes. (DTRs). Sensation was normal in all 4 patients. In the 4 patients with large disk involvement measured on pre-operative, MRI
all patients had normal motor, sensation and deep tendon reflexes.
Actual surgical volume of intervertebral disk size correlated with preoperative physical exam findings. None of the 3 patients with small surgical volume of intra-operative disk had any loss of motor, sensation or deep tendon reflexes measured preoperatively. Of the 5 patients with intra-operative disk volume being large, only 2/5 (40%) had decreased motor and deep tendon reflexes in the associated dermatome.
DISCUSSION
Lower back pain and radiculopathy from lumbar disk herniation (LDH) remains a common problem that presents to a myriad of physician specialties including family medicine, internal medicine, neurology and physical medicine and rehabilitation. In the absence of red flags such as a lower back trauma, neurologic deficit, signs of infection (fevers, chills) and concern for tumor (weight loss), then the first line treatment for a symptomatic LDH is conservative. Most authors recommend waiting at least 4-6 weeks before obtaining plan radiographs as many patient’s symptoms will substantially improve in this time period. Magnetic resonance imaging (MRI) is the gold standard imaging study for confirming a diagnosis of LDH and is typically reserved for patients with symptoms that have not improved with at least 4-6 weeks of dedicated conservative treatment. Surgical management in the absence of red flags, is reserved for patient with LDH with imaging-confirmed disk herniation with corresponding sciatic syndrome with significant symptoms that have not responded to 6-12 weeks of conservative management [5,6]. This study looked retrospectively at eight patients who underwent lumbar microdiscectomy for LDH and compared their pre-operative MRI disk size with their surgical disk size and their clinical signs & symptoms.
In this series, the size of the herniated disk on pre-operative MRI was not predictive of actual disk volume removed at the time of surgery 63% of the time. The ability of MRI to accurately assess disk herniation size, location and morphology has been substantiated [7,8]. There is a paucity of literature directly comparing the size of disk herniation pre-operatively on MRI to intra-operative size findings. However, a recent study suggested that more disk volume often needs to be excised in surgery than anticipated on MRI to ensure minimal or residual disk [9], hence preoperative MRI may underestimate how much disk needs to be removed to ensure adequate decompression.
This correlates with the current study in which preoperative MRI under-estimate actual surgical volume that was excised 38% of the time and was predictive of actual surgical volume removed only 37% of the time.
In respect to physical exam findings of motor strength; sensation and deep tendon reflexes, MRI volume did not correlate well. This study found that despite all patients having significant symptoms and failing conservative management, all 4 of the patients with large LDHs based on preoperative MRI had normal sensation, strength and DTRs. Furthermore, 2/4 (50%) of the patients with small LDHs on MRI had decreased motor strength in the correlative myotome and 2/4 (50%) had decreased DTRs in the correlative myotome. In this group with large LDH on MRI, all had normal sensation. It is often assumed that a larger lumbar disk herniation on MRI in itself is a risk factor for radiculopathy symptoms and physical exam findings. There is a growing body of literature suggestive that disk location, morphology, containment, enhancement with contrast and canal size are more correlative with radiculopathy symptoms and abnormal physical exam findings than purely just the presence of LDH and MRI disc volume [10-12].
Furthermore, presence and size of LDH on MRI does not
correlate well with patient symptoms or severity of symptoms.
Although MRI is the diagnostic gold standard for LDH, it is well established the presence alone of a LDH does not necessarily cause pain nor symptoms. MRI commonly shows herniated disks in asymptomatic individuals, with an increasing prevalence with age [7,8,13]. In his classic article, Boden et al. [14], 35% of subjects who were completely asymptomatic, had evidence of lumbar disk herniation on MRI. In this series, preoperative MRI volume alone was not predictive of preoperative symptoms. Half of the patients had small LDH on preoperative MRI and half had large LDH on preoperative MRI, yet all eight patients had significant radicular symptoms with frequent and debilitating pain.
In terms of surgical outcomes with discectomy in patients with LDH, lumbar disk herniation size on MRI has been found to have better surgical outcomes with larger disk herniations (>6 mm) [4]. However, this has been questioned in a recent study by En’Wezoh et al. [15] that questions this classic “6 mm” rule. The two major findings of their study were that although larger LDH may have better outcomes after surgery, there was no size threshold associated and that furthermore, preoperative factors such as functional scores had the largest effect on outcome. Although, compressive pathology concordant with patient’ s symptoms and physical exam findings is prerequisite for surgical interventions, outcomes after surgery for LDH are largely associated with psychological and social factors rather than imaging findings.
Several studies have found pre-operative psychological assessment highly predictive of outcome after surgery [16,17]. A classic study by Spengler et al. [18] looked at neurologic signs, clinical tension signs, psychological factors and imaging evidence of neural compression pre-operatively and found that although imaging studies were most predictive of operative findings, however it was pre-operative psychological score that best predicted outcome, not imaging findings. Abramovitz et al. [19] in a prospective comparative study had similar findings in that clinical examination and history, rather than MRI findings, could frequently predict outcomes for patients undergoing lumbar discectomies. More recent studies are increasingly emphasizing the importance of higher preoperative leg pain and low back pain severity and frequency, shorter symptoms duration and better mental health status as pre-operative factors predicting better outcomes after discectomy [20-22].
Given the findings of this study that MRI findings of disk size are not particularly correlative with patient symptoms, physical examination findings and actual surgical volume underscores the importance of appropriate ordering of advanced imaging, especially MRI. In the absence of red flags, there is growing evidence that early ordering of an MRI scan can have iatrogenic effects and may lead to unnecessary invasive procedures as well as patient anxiety. A 2013 study by Webster et al. [23] retrospectively assessed medical utilization, treatment and outcomes in patients with lower back pain with and without radiculopathy and whether their care included an MRI study that was ordered in adherence to evidence-based guidelines. These evidence- based guidelines recommend that an MRI should only be ordered in patients with red flags (severe trauma, infection, cancer, cauda equina) or in patients who had failed 4 weeks of conservative management and were healthy enough to be surgical candidates. They found an early MRI without an evidence-based indication, had a strong iatrogenic effect on patients care and higher cost and noted that “when early MRI is not indicated, it provides no benefits, and worse outcomes are likely.” There is a growing body of evidence that ordering an early MRI that is not adherent to evidence-based medicine results in increased medical care costs and interventions without improvement in outcomes at best, and likely will result in a worse outcome [24,25].
In this study the size of disk herniation based on pre-operative MRI was not correlative with symptoms, physical exam findings nor ultimate disk size at time of surgery. In the absence of contraindications to conservative management such as progressive neurologic compromise, cauda equina, infection and tumor, it is the opinion of the authors of this paper that the ideal surgical candidate for lumbar microdiscectomy would be a patient whose radicular symptoms are significant in terms of frequency and intensity in a pattern that is consistent with level of known lumbar disk herniation and has failed conservative management. Based on the findings in this study, the size of the disk herniation based on preoperative MRI findings is inconsistent with actual surgical volume, yet these patients experienced significant improvement in symptoms and had good surgical outcomes.
Limitations of this study include a small sample size, inability to objectively measure the exact volume of postoperative surgical pathology and retrospective nature.
CONCLUSIONS
Based on the author’s clinical experience, eight random surgical lumbosacral cases out of 80 lumbar microdiscectomies, one can conclude that preoperative MRI findings physical exam findings and disc size at the time of surgery does not correlate well with the probability of a good surgical outcome provided that there was no clinically significant psychological factors and functional issues. Frequency, duration, intensity and radicular pattern of pain in failed conservative treatment are more reliable predictors of surgical success.
REFERENCES
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581-585.
- Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine 1995;20(1):11-19.
- Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656-664.
- Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine.1997;22(14):1650-1660.
- Bhalla A, Bono CM, Schoenfeld AJ. Lumbar disc herniations. In: Garfin SR, Eismont FJ, Bell GR, et al. editors. The Spine. 7th ed. Philadelphia (PA) Elsevier. 2017;839-868.
- Deyo RA, Mirza SK. Clinical Practice. Herniated lumbar intertertebral disk. N Engl J Med. 2016;374:1763-1772.
- Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine. J 2014;14(1):180-191.
- Kim KY, Kim YT, Lee CS, Kang JS, Kim YJ. Magnetic resonance imaging in the evaluation of the lumbar herniated intervertebral disc. Int Orthop. 1993;17(4):241-244.
- Heo JH, Kim CH, Chung CK, Choi Y, Seo YG, Kim DH, et al. Quantity of disc removal and radiological outcomes of percutaneous endoscopic lumbar discectomy. Pain Physician. 2017;20(5):E737- E746.
- Komori H, Okawa A, Haro H, Muneta T, Yamamoto H, Shinomiya K. Contrast-enhanced magnetic resonance imaging conservative management of lumbar disc herniation. Spine. 1998;23(1):67-73.
- Ito T, Takano Y, Yuasa N. Types of lumbar herniated disc and clinical course. Spine. 2001;26(6):648-651.
- Mostofi K, Karimi Khouzani R. Reliability of the Path of the Sciatic Nerve, Congruence between Patients’ History and Medical Imaging Evidence of Disc Herniation and Its Role in Surgical Decision Making. Asian Spine J. 2015;9(2):200-204.
- Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol. 2015;36(4):811-816.
- Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-408.
- En’Wezoh DC, Leonard DA, Schoenfeld AJ, Harris MB, Zampini JM, Bono CM. Relationship between size of disc and early postoperative outcomes after lumbar discectomy. Arch Orthop Trauma Surg. 2017;137(6):805-811.
- Sorensen LV, Mors O, Skovlund O. A prospective study of the importance of psychological and social factors for the outcome after surgery in patients with slipped lumbar disk operated upon for the first time. Acta Neurochir (Wien). 1987;88(3-4):119-125.
- Barrios C, Ahmed M, Arrotegui JI, Björnsson A. Clinical factors predicting outcome after surgery for herniated lumbar disc: an epidemiological multivariate analysis. J Spinal Disord. 1990;3(3): 205-209.
- Spengler DM, Ouellette EA, Battie M, Zeh J. Elective discectomy for herniation of a lumbar disc: additional experience with an objective method. J Bone Joint Surg Am. 1990;72(2):320-327.
- Abramovitz JN, Neff SR. Lumbar disc surgery: results of the Prospective Lumbar Discectomy Study of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Neurosurgery. 1991;29(2):301-308.
- Oba H, Takahashi J, Tsutsumimoto T, Ikegami S, Ohta H, Yui M, et al. Predictors of improvement in low back pain after lumbar decompression surgery: prospective study of 140 patients. J Orthop Sci. 2017;22(4):641-646.
- Tschugg A, Lener S, Hartmann S, Ikegami S, Ohta H, Yui M, et al. Preoperative sport improves the outcome of lumbar disc surgery: a prospective monocentric cohort study. Neurosurg Rev. 2017;40(4): 597-604.
- Wilson CA, Roffey DM, Chow D, Alkherayf F, Wai EK. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016;16(11):1413-1422.
- Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine. 2013;38(22): 1939-1946.
- Webster BS, Choi Y, Bauer AZ, Cifuentes M, Pransky G. The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine. 2014;39(17):1433-1440.
- Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin GM. Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res. 2014;49(2):645-656.