Osseointegration for Amputees: Rationale and Evidence

Craig H. Lichtblau”1,2‘, Dror Paley’3, Stephen Quitman’s4, Christopher Warburtons5, Gabriel Meli6, Allyson7Gorman’ 1Physical Medicine and Rehabilitation Consultant to the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, FL, USA; 2Director of Rehabilitation for the Osseointegration Program Paley and Orthopedic and Spine Institute at St Mary’s Me4-41 Center, West Palm Beach, FL, USA; 3Director and Orthopedic Surgeon, Paley Orthopedic and Spine Institute at St. Mary’s Merl;e41 Center, West Palm Beach, Florida, USA; 4Orthoprwlic Surgeon, Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, Florida. USA; 5University of Miami Miller School of Medicine, Miami, FL, USA; 6Cornell University, Ithaca, New York, USA; 7Medical College of Wisconsin, Wauwatosa, WI, USA
ABSTRACT Amputees many times have significant difficulties from using socket prosthetic devices, which are associated with excessive weight and patient discomfort These patients suffer a poor quality of life and are in significant need of a superior alternative. Osseointegrated prosthetic implants, which are anchored to the bone, are proving superior to socket prostheses in many cases. Here we review the rationale and evidence for the value of osseointegration in amputees.
Keywords’ Osseointegration; Prostheses; Prosthetics; Socket prosthetic; Amputation; Amputee; Prosthesis; Phantom pain
INTRODUCTION
According to the World Health Organization, there are about 40 million amputees across the world [1]. By 2050, it is estimated that 3.6 million Americans will be living with the loss of a limb [2]. Although prostheses offer the potential to improve amputee function, conventional prostheses-referred to as socket prostheses-have failed to achieve optimal outcomes in a very large percentage of patients [2-4]. Socket prostheses are associated with poor range of motion, they lack stability, and they cause discomfort [5]. As a result, a high rate of prosthetic abandonment has been observed, with about one quarter of adults abandoning their body-powered and electric devices and pediatric patients abandoning these devices at rates of 45% and 35%, respectively [2]. Troublingly, data demonstrate that between one in three and one in four of those expressing significant dissatisfaction with their prostheses report that they consider themselves to have a poor or extremely poor quality of life [4,6]. It is thus critical that these patients are provided with a better alternative not only to sufficiendy restore functioning but also to improve their lives. Bone-anchored prosthetic implants, known as osseointegrated prosthetic implants have been developed over the past couple of decades to overcome the challenges posed by socket prostheses and provide a superior option for prosthetic patients [1,4,7-11]. Here we describe a demonstrative case study and provide the rationale and supportive evidence for the superiority of osseointegration over socket prostheses.
LITERATURE REVIEW
Osseointegration restores function and reduces pain in 21-yearold amputee Injurys On July 16, 2020, a 21-year-old ambidextrous female pedestrian was struck by a vehicle that had run a red light and suffe, crushing injuries to her left lower extremity in addition to other injuries to her right lower extremity. She was taken by ambulance to the local emergency department, where she received an emergency left above-knee amputation and a second revision surgery before being discharged from the hospital. Socket prosthesis On February 8, 2021, she sought our consultation after being wheelchair-bound (Figures 1 and 2). Her prosthesis weighed 10.7 pounds and caused severe pain in her
Correspondence to: Dr. Craig H. Lichtblau, Physical Medicine and Rehabilitation consultant to the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center, West Palm Beach, FL, USA, Email, clichtblau@chlmcLoom Received: 26-May-2022, Manuscript No. JPMR-22-17655; FAtror assigned: 30.•ay.2022, PreQC No. JPMR-22-17655 (PQ); Reviewed, 13-Jun-2022, QC No. JPMR•22-17655; Revised: 17-Jun-2022, Manuscript No. JPMR-22-17655 (R); Published: 27-Jun2022, DOI: 10.35248/2329-9096.22.10.632. Citations Lichtblau CH, Paley D, Quitman S, Warburton C, Meli G, Gorman A (2022) Osseointegration for Amputees: Rationale and Evidence. Int J Phys Med RehabiL 10:632. Copyright 0 2022 Lichtblau CH, et aL This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Lidatblau CH, et aL distal stump, rendering it useless to her. A physical examination revealed multiple neuromas in her residual left above-lmee stump. Her physical examination results are shown in Table 1. Targeted muscle reinnervation: The patient was admitted to a Level 1 Trauma Center on April 13, 2021. To restore functioning above the left knee stump, the orthopedic surgeon performed targeted muscle reinnervation on three nerves in the distal stump. The surgery was successful, and the patient healed without any complications, making her an ideal candidate for osseointegration.
Osseointegration: The patient underwent osseointegration on 08/17/2. Figure 3 shows the new implant The patient healed and during the postoperative period she developed a superficial skin infection that was treated with oral antibiotics without sequels. She had no other complications and participated in an outpatient rehabilitation program under direct medical supervision of a physiatrist The patient’s postoperative rehabilitation program included pre-prosthetic training and prosthetic training with a new custom fabricated prosthesis that was more than three pounds Lighter than her original socket prosthesis. The patient participated in the outpatient rehabilitation program and completed the program without any medical or surgical complications. Outcomes: Following the osseointegration procedure, patients tend to experience restored functioning and significant reductions in residual stump pain, including phantom limb pain. Donning and doffing the prosthetic device become much easier for the patient with the new prosthesis, and good osseo proprioception from ground reaction forces provides an improved gait and body mechanics in areas that had been compensating for loss of function. With improved body mechanics, patients often experience a significant reduction in lower back pain. Functional abilities usually improve, enabling amputees to ambulate independently and farther with prostheses that are attached with an osseointegration implant. The above example of osseointegration demonstrates a weight reduction in the patient’s original socket prosthesis from 10.7 pounds to 7.5 pounds, a reduction of 3.2 pounds with her new osseointegration prosthesis. In this example, the patient could not ambulate with her original heavy socket prosthesis, but following osseointegration, the lighter weight of her new prosthesis and the
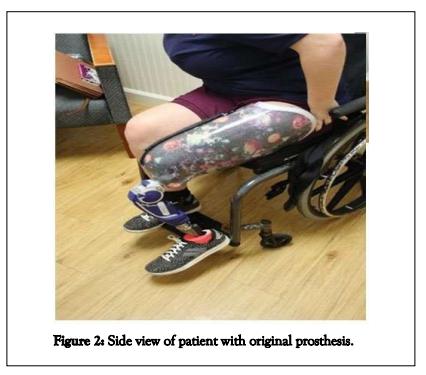

Table lt Patient’s physical examination results on February 8, 2021.
| Physical examination | Result |
| Constitutional (General): | WeRnourished, welkleveloped female. (Vital sign) Stable, afebrik. |
| Psychiatric | Alert and oriented x3. Short and longterm memory intact. Patient was in no acute distress. |
| Skin | The patient’s left above-knee stump was well-healed. No masses, lesions, discharge, or open areas. She was extremely painful to the touch and unable to wear her prosthetic device. |
| Extreraities | The patient has a left above Knee amputation. The residual limb has a welllealed scar with no open areas. ‘The patient has tenderness and exquisite pain to light palpation in her distal stump in the sciatic and femoral nerve distributions. |
| Gait | The patient was unable to ambulate with her current prosthesis due to pain in her distal stump and the weight of the prosthesis. |
Osseointegration superiority over socket prosthesesi The rationale and evidence
While this case study demonstrates how the limitations of socket prosthesis can be overcome through osseointegration, it is important to consider the specific weaknesses of socket prosthesis and strengths of osseointegration to understand the contexts in which osseointegration offers particularly high value to amputees. Socket prostheses often offer limited motor control and cause pain and discomforts Socket prostheses are associated with low satisfaction levels, which are the result of a combination of factors that limit the value of socket prostheses [1]. For instance, socket prostheses offer little limb proprioception and light touch sensation, which limit intuitive motor control [2]. In addition to difficulties with mobility, socket prostheses also cause pain and discomfort [4]. When asked about the problems they faced with their prostheses, survey respondents’ most common response was that they were bothered by heat or sweating in the prosthetic socket [4,12] They also commonly reported skin irritation and sores from the socket, difficulty walking, and pain in the residual limb. In addition to pain, poor socket fit can cause instability and local tissue damage [5,13]. It can also increase the stress on other parts of the body that work to compensate for the deficits associated with the lost limb and the prosthetic. These downsides of socket prostheses result from the nature of the technology. Residual volume changes, failure in load stability and transfer, and poor suspension are common challenges with socket-suspended prostheses [8]. Though the fit of the socket in the residual limb is critical for the success of the prosthesis, the dynamic nature of the residual limb makes fitting the stump-socket interface a significant challenge and can lead to the loss of even a well-established socket fit [4]. Complicating socket fit is that fitting a patient with a prosthetic socket requires manual work that is labor-intensive and lacks quantifiable information that could enable measuring and reporting on the fit [5].
Osseointegration overcomes challenges associated with socket prostheses: Osseointegration refers to the direct connection between the surface of a metal implant and living bone [4,14]. The technique was developed by Per-Ingvar Branemark and further refined by his son, Rickard Branemark [2]. Osseointegration-achieved direct skeletal fixation has been successfully used in a variety of applications induding dental implants, joint replacements, bone-anchored hearing aids, and ma3nllofacial reconstruction [4,9].

Lichtblau CH, et al.
The use of osseointegartion for attaching prosthetic limbs began in the 1990s and is beginning to be performed across the world to overcome the limitations of socket-based prostheses [14]. By attaching prostheses directly to the bone of the residual limb, the need for the socket interface and the challenges it presents are avoided [4,7-10,15,16]. Most of those who switch from traditional socket prostheses to osseointegrated ones show drastic improvements both objectively and subjectively [10]. These improvements have been demonstrated with tools including the Questionnaire for Persons with Transfemoral Amputation, Short Form-36 Physical Component Summary, 6 Minute Walk Test, and Timed Up and Go test [10,11].
The specific benefits of osseointegration over socket prostheses include
Better functioning and quality of life: Compared to socket prostheses, osseointegrated prostheses offer improved functioning and quality of life [4,15]. Specifically, those who undergo osseointegration tend to have improved walking proficiency, including the capacity to walk farther distances and for longer periods of time, owing to their ability to wear the prosthetic longer [15]. These patients are reported to have a more normal cadence and duration of gait cycle [10].
More limb sensation: Research on osseoperception, or the ability to identify a tactile stimulus that are transmitted via the bone-anchored prosthesis, has shown that perception is superior in osseointegrated prostheses than in socket prostheses [13]. Scientists interpret this finding to suggest that amputees with osseointegrated prostheses may have better kinesthetic awareness and be better able to respond to stimuli presented to their prosthetic limbs. Critically, unlike with other prostheses, people report that osseointegrated prostheses feel like a part of them [17]. This improved pressure and vibrotactile feedback is also associated with a greater freedom of motion [2,18-20].
Fewer abrasions and less pain: Unlike socket prostheses, osseointegration transfers energy directly to the skeleton and thus reduces abrasions [3]. Skin contact, tissue damage, and pain are minimized because the intramedullary metal implant attaches to the prosthetic via a small protrusion through the skin [131. In addition, reported sitting comfort has been shown to be improved [21].
Improved efficiency and durability when using myoelectric prostheses with osseointegration: Osseointegration improves device efficiency because it prevents challenges related to signal transduction between electrodes and myositis [2]. The survival rates of the prostheses are also impressive, with 2-year survival reaching between 92% and 95%. [3,22].
Improved efficiency and durability when using myoelectric prostheses with osseointegration: Osseointegration improves device efficiency because it prevents challenges related to signal transduction between electrodes and myositis [2]. The survival rates of the prostheses are also impressive, with 2-year survival reaching between 92% and 95%. [3,22].
Reduced energy requirements: Osseointegration reduces energy requirements compared to socket prostheses, making donning much easier [7]. The Physiological Cost Index (PCI) has been used to assess energy costs when patients walk with prostheses and has been deemed reliable for patients with lower-limb amputations [23]. The index provides a measure of extra heartbeats per meter of walking. Using this index, it has been shown that patients with osseointegrated prosthesis save more energy compared to those with socket prostheses. Research focused on oxygen requirements
bolsters this notion that osseointegrated prostheses are less energy intensive than the socket variety. These results have shown that the oxygen requirement associated with osseointegrated prostheses is 1,093 mL/min versus 1,330 mL/minute for socket prostheses [24]. Overall, the improved mobility and comfort that come with osseointegrated prosthetic devices increases patient satisfaction and prosthetic use, thus enhancing quality of life [8,10].
The future of osseointegration for amputees While osseointegration offers clear benefits to amputees, it is a relatively new procedure that suffers from some challenges. For instance, strategic planning and engineering must be implemented for each case of osseointegration to ensure the customized implant is the right size, and if the implant cannot be stably anchored to the bone directly, then the process must be aborted [3]. Osseointegration is associated with a few other risks as well.
Infection, fracture, and reoperation remain challenges in osseointegration
Risk for infection: Osseointegration is associated with an increased risk for soft tissue infection [1,8]. Most infections are caused by common organisms like staphylococcus aureus or coagulase-negative staphylococci and are superficial, resulting in pain, erythema, or discharge [111. Superficial infections are indeed the most common complication associated with osseointegration but have been shown to respond well to oral antibiotics [4]. Infections that require additional surgeries have been observed to have a risk of only 5% to 8% [10]. Nonetheless, human trials to evaluate the incidence of infection are ongoing [7]. Because the role of the skin is minimized with osseointegration, there is concern that patients may not benefit from the functional barrier that skin provides [13]. The lack of this layer of protection against the external environment may contribute to the increased risk of infection. In response to this concern, researchers are working to develop an environmental seal that could be incorporated into the osseointegration procedure.
Periprosthetic fracture and reoperation: Though there are clear advantages of osseointegration over socket prostheses, concerns have been raised about the potential for osseointegration to lead to cortical bone resorption around the implant, which could potentially cause outbreak fractures or aseptic loosening [15]. Reoperation may be necessary following osseointegration when excessive skin envelopes interfere with the prosthesis [9]. The stretching and loosening of tissues that occurs with time can also interfere with the prosthesis. It is therefore important to consider the soft tissue envelope when performing osseointegration for lower extremity amputations to avoid reoperation.
Ongoing clinical research will help to optimize osseointegration use in the future
Research on osseointegration has elucidated not only the general value and technical details of the procedure but also how the different versions of osseointegration-Branemark’s Osseo anchored Prostheses for the Rehabilitation of Amputees (OPRA) device and the Compress Transcutaneous Implant (CTI), and the Osseointegrated Prosthetic Limb (OPL) are particularly valuable for Lichtblaii CH, et aL patients whose soft tissue envelopes are compromised or who suffer short residual limbs [2]. The U.S. Food and Drug Administration Humanitarian Use Device designation for osseointegration is likely to spur even more research into the technique, and the resulting data will be invaluable in continually improving upon it and expanding its applications [4,10].
CONCLUSION
Though there are certain challenges associated with osseointegration, progress has been made to address and mitigate some of these issues. For instance, the strict rehabilitation protocols that were established in 1999 appeared to improve failure rates of osseointegrated prostheses. In 2009 when Branemark and Hagberg presented the results of 100 osseointegrated transfemoral prostheses, they revealed that most of the failure had occurred prior to 1999. Nonetheless, even for the challenges that remain, experts agree that these challenges do not occur at an unacceptably high rate nor are they insurmountable. In addition, as the U.S. Department of Defense is spearheading clinical trials in osseointegration, global interest is likely to increase in coming years, and patients and surgeons alike will benefit from forthcoming knowledge about the technique.
AUTHOR CONSENT
I give permission for images in which I appear to be used by International Journal of Physical Medicine & Rehabilitation for publications and public relations activities. I do not have any objection to upload my pictures in the article entitled ” Osseointegration for Amputees: Rationale, Evidence”. In particular, I note that this may include use in print and electronic media, including the Internet and official social media platforms. I have read and understand this notice, and consent to the collection, use and disclosure of my image, including disclosure to overseas recipients, as outlined.t.
REFERENCES
- Patera L, Ibrahimi M, Gruppioni E, Menciassi A, Ricotti L Sockets for limb prostheses: a review of existing technologies and open challenges. IEEE Trans Biomed Eng. 2018;65(9):1996-2010.
- Bates TJ, Fergason JR, Pierrie SN. Technological advances in prosthesis design and rehabilitation following upper extremity limb loss. Current Rev Musculoskelet Med. 2020;13(4):485-93.
- Hoellwarth JS, Al Muderis M, Rozbruch SR. Cementing osseointegration implants results in loosening: case report and review of literature. Cureus. 2020;12(2).
- Hebert JS, Rehani M, Stiegelmar R. Osseointegration for lower-limb amputation: a systematic review of clinical outcomes. IBIS Rev. 2017;5(10):e10.
- LaPrB AK, Nguyen VQ, Baspinar U, White M, Sup FC. Capturing prosthetic socket fitment: Preliminary results using an ultrasound-based device. In2017 Int Conf Rehabil Robot 2017; 1221-1226.
- Pezzin LE, Dillingham TR, MacKenzie EJ, Ephraim P, Rossbach P. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil. 2004;85(5):723-9.
- Kistenberg RS. Prosthetic choices for people with leg and arm amputations. Phys Med Rehabil Clin N Am. 2014;25(1):93-115.
- Kunutsor SK, Gillatt D, Blom AW. Systematic review of the safety and efficacy of osseointegration prosthesis after limb amputation. Br J Surg. 2018;105(13):1731-41.
- Marano AA, Modiri 0, Rozbruch SR, Otterburn DM. Soft tissue contouring at the time of osseointegrated implant reconstruction for lower extremity amputation. Ann Plast Surg. 2020;85(S1):S33-36.
- Hoellwarth JS, Tetsworth K, Rozbruch SR, Handal MB, Coughlan A, Al Muderis M. Osseointegration for amputees: current implants, techniques, and future directions. JBJS reviews. 2020;8(3).
- Overmann AL, Forsberg JA. The state of the art of osseointegration for limb prosthesis. Biomed Eng Lett. 2020;10(1):5-16.
- Hagberg K, Branemark R. Consequences of non-vascular trans-femoral amputation: A survey of quality of life, prosthetic use and problems. Prosthet Orthot Int 2001;25(3):186-94.
- Laferrier JZ, Gailey R. Advances in lower-limb prosthetic technology. Phys Med Rehabil Clin N Am. 2010;21(1):87-110.
- Lichtblau C, Hennekens CH. Osseointegration: A Novel Technology for Amputees. Int J Phys Med Rehabil. 2018;6(5):48
- Haket LM, Fralke JP, Verdonschot N, Tomaszewski PK, van de Meent H. Periprosthetic cortical bone remodeling in patients with an osseointegrated leg prosthesis. J Orthop Res. 2017;35(6):1237-41.
- Mioton LM, Dumanian GA. Targeted muscle reinnervation and prosthetic rehabilitation after limb loss. J Surg Oncol. 2018;118(5):807-14.